For Some, Finding A Match Is About Life And Death

Can artificial intelligence help underpin the gross undersupply of organ transplants?
At 2 AM, Emily was suddenly awakened by the buzzing of her phone. A prisoner of end-stage renal disease, a kidney transplant was her only chance at freedom. After an agonizing two years, her surgeon had called to inform her of a possible kidney match. But he had reservations. His gut said she needed a better-quality kidney. And just as fast as she had reached for her phone seconds ago, Emily found herself back on the waitlist.
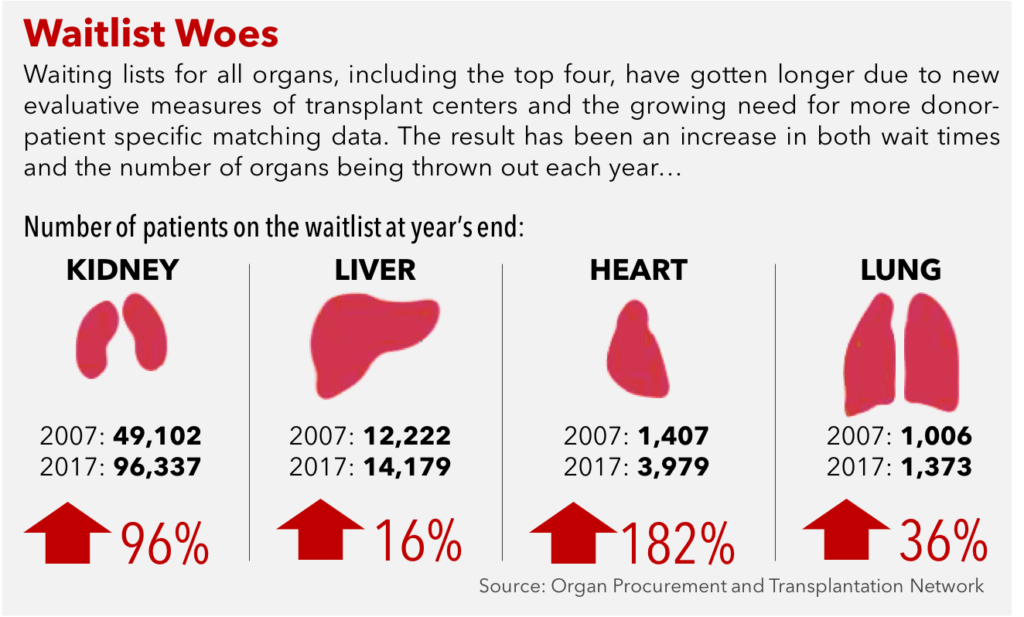
Emily is just one of approximately 117,000 patients currently in need of a lifesaving organ transplant [1]. In a dire scenario where current demand outstrips supply, nearly 7,000 patients die every year while another 3,000 become too ill for transplant waiting for their match [2]. In 2017, there have been only 12,211 donors contributing 26,034 transplants, a far cry from what is required to clear the backlog [1]. Despite numerous efforts from policymakers and public marketing campaigns to increase the registry of organ donors, the wait list continues to grow disproportionately to the number of transplants being performed each year [2].
Tackling this challenge is United Network for Organ Sharing (UNOS), a non-profit organization responsible for allocating available organs to waitlisted patients in the U.S. With the digitalization of medical information, UNOS now relies on an internet-based system called DonorNet, which compares data between the donor and the patient, including weight, blood type, and geographical location. The algorithm tries to objectively rank viable patients based on illness and likelihood of a successful outcome. In UNOS’s ideal scenario, every viable organ is transplanted to a waitlisted patient.
But like with many critical decisions, subjectivity creeps in. For the sake of equality, UNOS’s current matching system disregards ethnicity, gender, and financial status [3]. Yet, these are critical factors that can impact organ transplant success [4]. As a surgeon evaluates the DonorNet results, she must ultimately resort to experience and intuition to accept or decline the available organ [5, 6]. Unfortunately, experience-based “algorithms” are subject to the inexactitudes that afflict anecdotal decision-making. Recent studies have shown that utilization of the existing supply is poor, with donor organ discard rate exceeding as much as 40 percent in some instances [7, 8, 9]. It’s at this intersection of quasi-numerical assessment of a patient’s health factors and gut instinct where intelligent exploration of large datasets of patient characteristics and organ supply cycles can assist in this complex decision-making process.
Overwhelmed by the ambiguity and diversity of relevant data, UNOS has been slow to restructure its allocation algorithms. In 2014, after spending nearly 10 years feuding between surgeons, patient advocates, and policymakers, UNOS released a revised metric for kidney allocation [10]. In an effort to make access more equitable and increase the utilization of kidneys, UNOS digitized a continuous stream of data, integrating time on dialysis, current diabetes status, and whether the candidate had a previous organ transplant [3]. Although there has been a moderate increase in procedures, the procurement of donor organs as well as the discard rate has seen little to no improvement [11, 12]. Under its current system, DonorNet will require years of data collection before an appropriate evaluation can be done. It seems prudent, then, that UNOS continue to increase transparency of available organs and reduce lead times for existing supply to incrementally increase utilization.
But what if DonorNet could provide a more holistic likelihood of success based on qualitative factors like ethnicity and income level? And what if DonorNet could know exactly how long, if a patient passes her turn on the list, has to wait for an optimal donor? This is where artificial intelligence (AI) can help UNOS breakthrough its supply-demand problem in the long run. With advances in supercomputing to filter and process millions of indiscernible data points, UNOS can leverage AI to make DonorNet a forward-looking decision-making tool rather than rely solely on backwards-looking data.
Researchers have already begun to evaluate the feasibility of machine learning for organ allocation, demonstrating the accuracy of model estimations of up to 87% [6]. In an effort to illicit patterns from millions of past clinical decisions, surgical outcomes, and patient demographics, AI-based algorithms are beginning to provide insights that would give DonorNet the capability to provide patients and surgeons highly comprehensive decision metrics based on macro-level trends that are nearly impossible to study based on current techniques.
But how far can UNOS take DonorNet to completely change surgeon behavior? And what are the ethical boundaries that UNOS would be responsible for to curtail the level of AI decision making power? And if downstream supply continues to lag, will enhanced organ utilization make the system truly more efficient? For now, the hope is that such a model will eventually reduce the rate of discarded organs and give patients like Emily the chance to live another day.
(800 words)
References
[1] Unos.org. (2017). Data | UNOS. [online] Available at: https://unos.org/data/
[2] 2015 Annual Data Report. Scientific Registry of Transplant Recipients http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx
[3] Organ Procurement and Transplantation Network (n.d.). The New Kidney Allocation System (KAS) Frequently Asked Questions. [online] Available at: https://optn.transplant.hrsa.gov/media/1235/kas_faqs.pdf
[4]Morris, Alanna A., Andreas P. Kalogeropoulos, Liping Zhao, Melissa Owen, S. Raja Laskar, J. David Vega, Andrew Smith, and Javed Butler. 2015. “Race And Ethnic Differences In The Epidemiology And Risk Factors For Graft Failure After Heart Transplantation”. The Journal Of Heart And Lung Transplantation 34 (6): 825-831. doi:10.1016/j.healun.2014.12.012.
[5] (2017). How an analytics-based predictive model can improve kidney transplant survival rates. http://mitsloan.mit.edu/newsroom/articles/how-an-analytics-based-predictive-model-can-improve-kidney-transplant-survival-rates/
[6] Bertsimas, D., Kung, J., Trichakis, N., Wojciechowski, D. and Vagefi, P. (2017). Accept or Decline? An Analytics-Based Decision Tool for Kidney Offer Evaluation. Transplantation, p.1
[7] B. Tanriover, S. Mohan, D.J. Cohen, et al., Kidneys at higher risk of discard: expanding the role of dual kidney transplantation, Am. J. Transplant. 14 (2014) 404–415.
[8] Yasinski, E. (2017). When Donated Organs Go to Waste. [online] The Atlantic. https://www.theatlantic.com/health/archive/2016/02/when-donated-organs-go-to-waste/470838/
[9] Stewart, D., Garcia, V., Rosendale, J., Klassen, D. and Carrico, B. (2017). Diagnosing the Decades-Long Rise in the Deceased Donor Kidney Discard Rate in the United States. Transplantation, 101(3), pp.575-587.
[10] Wang, C., Wetmore, J. and Israni, A. (2017). Old versus new: Progress in reaching the goals of the new kidney allocation system. Human Immunology, 78(1), pp.9-15.
[11] Organ Procurement and Transplantation Network, The New Kidney Allocation System: The First Year, 2016.
[12] Organ Procurement and Transplantation Network, Analysis Shows Kidney Allocation System Achieving Goals, 2016.



The notion that organs are discarded at a 40% rate is quite shocking and saddening. However, I’m curious what percentage of this waste is due to inadequate ability to predict transplant success (the problem that AI would solve). For instance, if some of the waste is due to geographic mismatch in supply and demand, there is little AI could do. (This seems likely, as certain regions have so many fewer organ donors that the average wait for a transplant is 6x longer than in other regions.) Another explanation might relate to poor incentives for doctors: doctors are judged based on the 1-year survival rate of patients they choose to operate on; therefore, patients they chose not to operate on are not incorporated into their accountability metrics. This potentially gives an incentive to reject “good fit” organs for high risk patients. Even if an AI algorithm could correctly identify good matches, so long as the doctor makes the ultimate decision to operate or not, they will be incentivized to not operate on risky patients. In all, this seems like an area that is ripe for AI to have some impact, but in which AI will need to be paired with other reforms, including marketing and governance changes, in order to be effective.
Thank you for a very interesting article. It hurts me that there are so many people who need organ transplant but can’t get it. I agree with you that AI would make transplant much successful. However, I feel like this is more of a supply and demand issue where there is a lot more demand vs. supply. I believe that UNOS needs to initially focus on getting people to donate more organs so that demand can be met. They can do so by doing marketing, incentivizing people to donate more, etc. Then, AI can help surgeons decide which organ for which patient. However, as dgoldberg mentioned above, surgeons may be making decisions that would be the best interest for them. I think this is another area AI can contribute by being objective and solving for patients and surgeons both.
Really interesting. I’d be curious how the relevance and feasibility of an AI sorting algorithm differs between organ types. Some organs have many fewer numbers of transplants per year than others and may lack the large datasets needed for machine-learning algorithms. It seems that AI could be a very useful tool, but not a panacea across the board – at least at current rates of donation.
I agree that we should also be working to increase the supply of donations, which would help solve the problem and also increase the value of an AI sorting algorithm. One simple fix would be to have an opt-out rather than an opt-in system. Many European countries use the opt-out system, in which citizens are by default treated as organ donors unless they choose to opt-out. By contrast, in the United States, you have to voluntarily opt-in to become an organ donor. The opt-out system leads to a much higher percentage of the population donating their organs – which ultimately saves lives.