RubiconMD: Treating Referrals

Tackling referrals and healthcare's triple aim
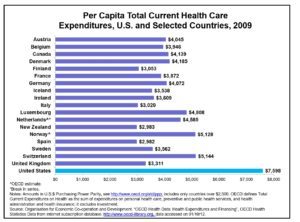
Two of the primary drivers for health reform in the U.S are rapid increases in health care spending and concerns about quality of care. In 2012, The Institute of Medicine estimated that roughly $750 billion,[i] about 30% of health care spending, was wasted.
A microcosm for the inefficiency seen in the larger health system is seen in the current referral process. Typically, the primary care provider (PCP) makes the decision to refer to a specialist. Surveys of both PCPs and specialists have shown dissatisfaction with the current referral system.[ii] Inappropriate referrals, which by some estimates account up to 65% of all referrals,[iii] often emerge from adequate communication between PCPs and specialists. This poor communication often leads to duplicate and unnecessary tests as well as fragmented care[iv], [v]. Contributing heavily to the wasted spending and inefficiency in the current referral process are the duplicate and unnecessary tests, and the fragmented care such as records not being available at time of appointment, avoidable repetitive visits, and receiving differing information from various professionals. Moreover, the poor communication in the referral process can lead to adverse outcomes,[vi] physician dissatisfaction,[vii] and delayed diagnosis.
Figure 1: Triple aim of healthcare
(source: phrazer.com)
Figure 2: Per capita healthcare expenditures by country 2009
Some studies have estimated that over 30% of referrals could be avoided in their entirety if other lines of communication between PCPs and specialists were present.[viii] RubiconMD is a health IT venture that connects general practitioners to top specialists for remote opinions via a HIPAA compliant web platform, allowing the PCP ask general or patient-specific questions to specialists remotely and receive answers or guidance over a web and email platform. This online asynchronous eReferral can almost be viewed as a as a supplement or alternative to the “curbside” consult. The curbside is when PCPs and specialists interact in informal settings such as hospital hallways and have talks or mini-consults regarding their patients. However, these interactions rely on incidental contact and either close physical proximity between providers or easy phone access.
By receiving specialist input on cases, general practitioners can then make more informed decisions on the diagnosis and management of their patients. In addition to improved clinician satisfaction and education, RubiconMD generates value for all parties involved in healthcare delivery:
Reduced Costs – Unnecessary specialist referrals are reduced and unnecessary services are minimized. Most estimates show a reduction in specialist referrals by 30%.[ix]
Improved Care Coordination – The patient remains with their PCP who is typically more familiar with them and their case. If a patient is referred out, they are done so with the correct tests at the appropriate time with the right type of specialist.
Earlier Specialist Opinion – One study found that Medicaid patients had to wait twice as long for high-demand specialists with appointment wait times ranging from 48-103 days.[x] Typically eReferrals have a much quicker turnaround time: at the Mayo Clinic, the time frame for a virtual consult was 1 day, 6 hours compared to 7 days, 20 hours for a traditional consultation.[xi]
Increased Patient Satisfaction – Patients receive quicker responses from specialist, have less hassle with scheduling appointments, and often have a reduced total cost.
Although multiple payment models exist based on the type of insurance risk-sharing plan, generally RubiconMD specialists are paid per consult, of which RubiconMD takes a piece of. As discussed above, the company has done an excellent job of generating value for multiple parties in the health care chain through novel technology. I believe an important next step from a technology perspective is broader integration into electronic health records to incorporate the technology into clinician workflow.
Word Count: 798
References:
[i] Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press, 2013.
[ii] T. Bodenheimer, “Coordinating Care—A Perilous Journey Through the Health Care System,” New England Journal of Medicine, March 6, 2008 358(10):1064–71.
[iii] A. Mehrotra, C. B. Forrest, and C. Y. Lin, “Dropping the Baton: Specialty Referrals in the United States,” Milbank Quarterly, March 2011 89(1):39–68.
[iv] Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15(9):626–631. doi: 10.1046/j.1525-1497.2000.91119.x.
[v] Epstein RM. Communication between primary care physicians and consultants. Arch Fam Med. 1995;4(5):403–409. doi: 10.1001/archfami.4.5.403.
[vi] Levin A. Consequences of late referral on patient outcomes.Nephrol Dial Transplant. 2000;15(Suppl 3):8–13.
[vii] Wood ML. Communication between cancer specialists and family doctors. Can Fam Physician. 1993;39:49–57.
[viii] M. T. Donohoe, R. L. Kravitz, D. B. Wheeler et al., “Reasons for Outpatient Referrals from Generalists to Specialists,” Journal of General Internal Medicine, May 1999 14(5):281–86.
[ix] Harno, “UUMA. Regional eHealth Services,” 2004 and Patterson, Humphreys, and Chua, “Email Triage,” 2004.
[x] Bisgaier J, Rhodes KV. Auditing access to specialty care for children with public insurance. N Engl J Med. 2011;364(24):2324-33.
[xi] K. B. Angstman, S. C. Adamson, J. W. Furst et al., “Provider Satisfaction with Virtual Specialist Consultations in a Family Medicine Department,” The Health Care Manager, Jan.–March 2009 28(1):14–18.



Ryan – this was a really interesting article and company – I love how they are making the “hand-off” and diagnosis process more efficient.
One thing I was curious about was the pricing model for RubiconMD. You mentioned that specialists receive a payment per consult. I wonder if there is an equilibrium price point where we can solve for key areas of potential tension. For example: 1) specialists, if they make too much on RubiconMD, will spend more time on this online platform and less time with in-person patients (which I would argue would decrease overall quality of healthcare) and 2) specialists, if they aren’t paid enough, won’t join the platform. After all, the availability of online consultants via RubiconMD could decrease the overall pie of people who need to see specialists (and hurt specialists’ offline business). Although specialist demand typically far exceeds specialist supply, I am also worried about rural specialists with less demand – will this alienate them? If specialists are spending all their time on the RubiconMD platform, will this just make the demand > supply problem worse?
Really interesting article Ryan. To be honest, I’m surprised it’s taken Rubicon (or competitors) so long to come up with the platform. Seems like a no brainer: adding a ton of value to all players in the healthcare system. I completely agree with your last line re: integration of electronic medical records. Improvements in electronic data collection, storage and usage capability will also lead to improved PCP effectiveness, general population health and cost of care. The improvement in population health through electronic data collection is most intriguing to me personally. There is a big data company called Opera Solutions (https://www.operasolutions.com) that is doing some very interesting thins with electronic medical records — they’re working with hospitals systems across the country to gather data on cancer treatment choices and survival rates in an attempt to better optimize treatment for patients based on age, history of health, etc.
Thanks for the article Ryan – seems like an interesting problem to tackle. My biggest question would be how an asynchronous interaction compares with the curbside consult in terms of efficiency and efficacy. Realize that the curbside consult has the obvious drawback of access, but isn’t it much easier to communicate in person vs. over email, especially in time-sensitive and complex situations?