Practice Fusion: Electronic Health Records (EHR) Now FREE…

Looking at the digitization of medical records and future potential.
It’s hard to believe that as recently as 2012 the majority of our medical records were stored physically in the form of hand written records (United Sates). It seems a bit primitive given the massive leaps medical technology has made in the past 25 years. To put things in perspective, the first heart transplant occurred in 1967 [4]. Having good electronic records seems like simple idea in comparison. Enter Practice Fusion, an entrepreneurial company which is provides them for free…
What is an EMR?
Electronic Health Records (EHRs) provide a comprehensive patient health history. These records are the complete set of medical and clinical data gathered during a patient’s life across all providers they have visited. An EHR is intended to be used by anyone involved in a patient’s care. It can only be modified by authorized users. EHRs unlike Electronic Medical Records (EMR) can move with the patient anywhere they go. An EMR is simply a digital version of a paper chart that has a patient’s history from just one provider.
Benefits of Digitizing Health Records
Your car has a maintenance history, which now almost entirely digitized, automated and distributed to a network of dealers which can provide servicing. Why shouldn’t your body have the same privilege?
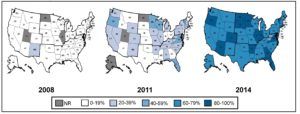
Basic EMR Penetration Amongst Acute Care Hospitals [4]
EHRs provide you the ability to track data and valuable biometrics over time. They identify and automatically notify you when you are due for preventative visits and screenings. EHRs will continuously monitor your vaccination status. The benefits have driven the adoption of this technology as shown above.
Practice Fusion is taking the idea one step further and putting everything on the cloud to improve accessibility and automatic updating. The system allows physicians to chart on any device [5].
Additionally, the creation of an EHR provides massive amounts of potential to have various systems connect. Billing, scheduling and task management can all be incorporated into the patients file to coordinate care and consolidate provider and staff responsibilities. Practice Fusion also provides intuitive charting based on data collected to assist physicians in making assessments about patient health. The Practice Fusion EHR has also been ranked as the number one e-prescribing system. By integrating prescriptions, drug to drug interactions and drug-allergy interactions are automatically reverified incase the physician misses something. The system can also help reduce out of pocket costs by searching the web for eCoupons [5].
Diagnostic tests, imaging and x-rays can all be imported in the EHR to allow both the physician and patient to access the same data, thereby improving communication and transparency. If a primary care physician refers you to a specialist, they will automatically record of all the visits and tests done to date.
Hospitals have massive financial upside by implementing good integrated EHR systems. For the points mentioned, utilization of physicians, nurses and lab techs can be improved [1]. Information flow will assist all health practitioners to make better decisions. Integrated scheduling will improve utilization of expensive imaging equipment and prevent unnecessary work to be reperformed.
From the patient perspective, the experience is massively improved. Before the visit, a patient will get a confirmation and reminder of any pre-appointment procedures to follow. During the visit, additional clinical brochures and pamphlets can be accessed to better explain certain conditions. Finally, after the visit patients can continue to log in and see their own health data with any recommended action items from their doctors.
Risks
The primary reason EHRs have taken so long to implement is due to the sensitivity of the data. Health records have strict regulations (HIPAA) which mandate how certain healthcare transactions can occur electronically. It also sets limits and conditions on the uses and disclosures that may be made of data without patient notification [6].
Additionally, with implementation of any new system there are new logistical challenges. Hospitals have standardized workflows which have been designed around the traditional method of hard copy record taking. With implementation of electronic history logging there are new challenges around work flows which may need to be redesigned.
The Future
EHRs have made great progress but applications are unlimited. Imagine carrying your entire personal history on your phone. In an emergency, anyone treating you can easily know of your pre-existing conditions, any allergies to medicines etc., and can avoid costly errors. New data that is actively being captured from your wearable device can show up on your doctor’s dashboard if any vitals are out of safe limits. Further information can be incorporated with a “Therable”, therapy delivering wearable. Imagine a diabetic who is wearing a smart watch that can actively monitor and deliver insulin as needed. Hospitals, insurers and consumers all have a role to play in thinking about the applications of digitization on the cost and quality of care during our lives.
Sources
[1] http://reports.weforum.org/industrial-internet-of-things/executive-summary/
[2] http://columbiasurgery.org/heart-transplant/brief-history-heart-transplantation
[3] https://www.healthit.gov/providers-professionals/electronic-medical-records-emr
[4] https://www.healthit.gov/sites/default/files/data-brief/2014HospitalAdoptionDataBrief.pdf
[5] http://www.practicefusion.com/electronic-health-record-ehr/
[6] https://www.hhs.gov/hipaa/for-professionals/privacy/



This is a really well written and interesting post, Sho-time, thanks for sharing! Your comment on the hospitals saving money was an interesting one, I had not thought through EHRs thoroughly enough to understand that the utilisation of the hospital staff would increase after the EHRs had been implemented and the staff trained. However, as you correctly stated in the “risks” section of your post, there are logistical challenges with implementing a new system within any organisation and one, such as a hospital, where every second costs money and every second could be critical in saving a person’s life. I wonder if hospitals are at a point where they have the flexibility to be able to choose to implement a new system.
As well, utilisation of healthcare staff will drop significantly as the new system is implemented and, as we saw in the FIN case on Partners Healthcare, the margins in hospitals are often as low as 3% per annum, not leaving any room for error or disruption within the system. This Hospital Report shows Operating Margins at 2.6% for the hospital. (http://www.beckershospitalreview.com/lists/200-hospital-benchmarks-2015.html). Do you think that although there are significant upsides to hospitals switching to EHRs tat perhaps established hospitals are not at a place where that is possible and instead we should focus on implementing and teaching this in medical schools to the next generation of healthcare professionals, and implement it in new hospitals, and have that be the way that we start to integrate it into our medical world? The other alternative, that perhaps might be more effective, is to require that all hospitals switch over at a certain point and have emergency services on hand to accommodate for the dip that there will be in outcome and productivity, though this does not deal with the financial risks and how insurance might perceive any errors made by the healthcare staff during this time. I would love to know what you think.