Myth or Reality: Exploring the Potential for Machine Learning to Improve Care Delivery in the UK’s National Health Service
Machine-learning driven advancements in healthcare have promised much but left us waiting. Will the UK National Health Service's latest effort fare any better?
Machine learning could play an important and much-needed role in improving care delivery
The UK’s 70-year-old National Health Service (NHS) was founded with the aim of providing universal healthcare free at the point of use (1). However, the dual challenge of increased demand and constrained capacity challenged those founding principles. Long-term conditions; multi-morbidity; an ageing population and rising patient expectations have pressured the system. By 2020/21, the NHS predicted a funding gap of £30 billion per year (2).
Machine learning techniques can solve problems across the spectrum of care: from risk stratification and population health management; diagnosis and treatment selection to prognostication. Unfortunately, despite the earlier optimism, machine learning has not had the anticipated impact in medicine (3).
In November 2018, the NHS announced £50m of funding to create 5 centers of excellence in the UK dedicated to using machine learning techniques in medical imaging for pathology and radiology (4). However, it is not clear if this latest push will deliver on the machine learning driven breakthrough in medicine we have been waiting to see.
To drive a step-change in performance, machine-learning based healthcare solutions must be: i) Specific in-scope and address problems well-suited to machine learning ii) Reliant on data that is structured and accessible iii) Focused on tackling key barriers to adoption.
i) Specific in-scope and address problems well-suited to machine learning
Machine learning techniques are well-suited to improving diagnosis in radiology and pathology (5). In radiology, there are several impressive use cases for machine-learning. Algorithms can already replace a second radiologist in reading mammograms, dramatically improving radiologist productivity (6). In pathology, some deep learning algorithms submitted as part of the researcher challenge competition (CAMELYON16) achieved better diagnostic performance than a panel of expert pathologists (7). The availability of digital images that can easily be used to train algorithms makes machine learning well-suited to these specialities.
ii) Reliant on data that is structured and accessible
Machine learning algorithms are very data-dependent, often requiring millions of observations to reach acceptable performance levels (8). Biases in data collection can substantially affect both performance and generalizability. For example, in medicine, high lactate levels may be a strong predictor of the risk of death, but only a small and unrepresentative sample (the seriously ill) have this level checked (5).
In 2017, the University of Texas M.D. Anderson Cancer Center in Houston let its contract with IBM Watson expire before the system was used on any patients, despite 5 years of development and $62m invested (9). Unstructured data and language processing was a major challenge. In clinical notes, Watson could not reliably distinguish the acronym for acute lymphoblastic leukaemia, ALL, from the shorthand for allergy, also ALL – a feat which no junior physician would struggle to accomplish.
iii) Focused on tackling the major barriers to adoption
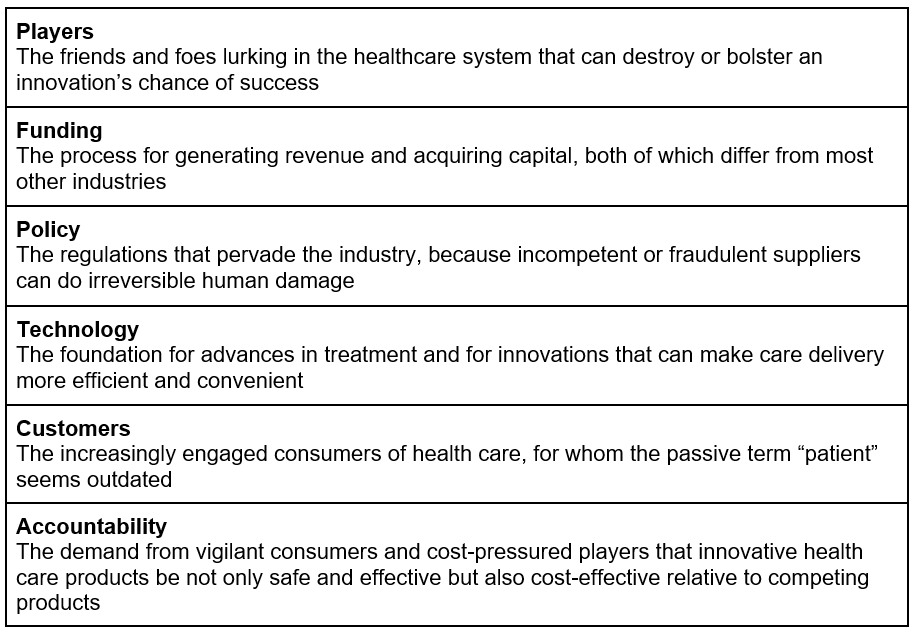
Driving adoption of machine-learning solutions by clinicians is difficult, particularly when the emphasis is on a man versus machine, rather than a man aided by machine narrative. When minimally invasive surgery techniques were first introduced, surgeons resisted their adoption despite the potential benefits to patients (10). Innovators in machine learning must reflect on the role of physicians as a major gatekeeper to adoption, whilst also adapting their models around the six factors that can drive or kill healthcare innovation (Table 1).
So far, the NHS is taking the right steps to accelerate adoption of machine-learning solutions, but there are other areas to consider
The NHS promotes machine-learning through both medical imaging (via the recently announced five national centers) and other AI bets. As one of its bets, the NHS is exploring the potential of machine-learning powered care-navigation and triage tools. Sense.Ly’s Ask NHS App uses machine learning to drive its clinical decision support technology (11). Babylon Health’s GP at Hand App, provides a symptom checker for patients, but the service is controversial, claims that it met the standard to pass doctor licensing exams are refuted by some researchers (12,13).
The UK should take care in allocating resources to those opportunities which are best suited to machine learning techniques. The focus of the national centers on imaging in radiology and pathology seems more appropriate than some of the other machine learning bets, which are less well proven in the short-term.
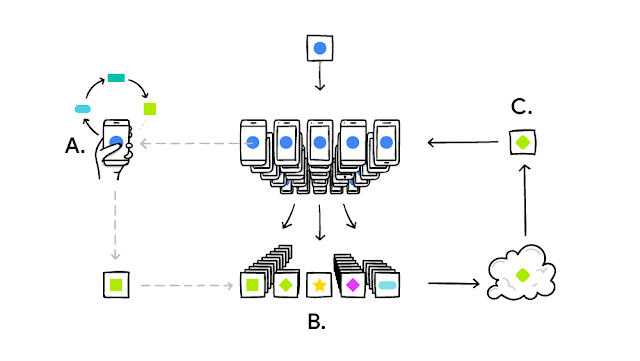
The NHS is focused on improving access to data, a goal which it should continue. One of the national centers will create a data lake for pathology images (14). Going forward, the NHS should continue to improve access to data and consider newer techniques like federated learning to overcome the barriers to data-sharing (15). Efforts should also be made to align normal clinical practice with structured data collection, such as deliberate investments in enabling IT infrastructure.
In the longer term, focus should be placed on tackling barriers to adoption by physicians. Stakeholders should consider formal roles for which physicians may be well suited, e.g. as product managers roles and clinical advisors. Strong consideration should be put to the evidence base required before solutions are deployed, to maximize patient and physician confidence.
Open questions
- Beyond medical imaging, what other high-potential areas should the NHS consider?
- How else can the NHS tackle key barriers to adoption?
(799)
References
- Iacobucci G. A service under pressure. BMJ. 2017 Jan 3;356:i6691.
- NHS England » NHS Five Year Forward View [Internet]. [cited 2018 Nov 11]. Available from: https://www.england.nhs.uk/publication/nhs-five-year-forward-view/
- Ramesh AN, Kambhampati C, Monson JRT, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004 Sep;86(5):334–8.
- Artificial Intelligence to help save lives at five new technology centres [Internet]. GOV.UK. [cited 2018 Nov 12]. Available from: https://www.gov.uk/government/news/artificial-intelligence-to-help-save-lives-at-five-new-technology-centres
- Obermeyer Z, Emanuel EJ. Predicting the future—big data, machine learning, and clinical medicine. N Engl J Med. 2016;375(13):1216.
- Gilbert FJ, Astley SM, Gillan MG, Agbaje OF, Wallis MG, James J, et al. Single reading with computer-aided detection for screening mammography. N Engl J Med. 2008;359(16):1675–1684.
- Bejnordi BE, Veta M, Van Diest PJ, Van Ginneken B, Karssemeijer N, Litjens G, et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. Jama. 2017;318(22):2199–2210.
- Halevy A, Norvig P, Pereira F. The unreasonable effectiveness of data. IEEE Intell Syst. 2009;24(2):8–12.
- Schmidt C. M. D. Anderson Breaks With IBM Watson, Raising Questions About Artificial Intelligence in Oncology. JNCI J Natl Cancer Inst [Internet]. 2017 May 1 [cited 2018 Nov 12];109(5). Available from: https://academic.oup.com/jnci/article/109/5/djx113/3847623
- Herzlinger RE. Why innovation in health care is so hard. Harv Bus Rev. 2006;84(5):58.
- One Health Lewisham signs deal for virtual assistant app [Internet]. Digital Health. 2018 [cited 2018 Nov 12]. Available from: https://www.digitalhealth.net/2018/05/one-health-lewisham-virtual-assistant-app/
- Cellan-Jones JC Rory. Chatbot claims to beat GPs at medical exam. 2018 Jun 27 [cited 2018 Nov 12]; Available from: https://www.bbc.com/news/technology-44635134
- Safety of patient-facing digital symptom checkers – The Lancet [Internet]. [cited 2018 Nov 12]. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32819-8/fulltext
- Warwick awarded £2.3 million to help develop cutting-edge technologies for cancer diagnosis and personalised treatment [Internet]. [cited 2018 Nov 12]. Available from: https://warwick.ac.uk/newsandevents/pressreleases/warwick_awarded_23/
- Federated Learning: Collaborative Machine Learning without Centralized Training Data [Internet]. Google AI Blog. [cited 2018 Nov 12]. Available from: http://ai.googleblog.com/2017/04/federated-learning-collaborative.html
- Berlin L. Archive or Discard Computer-Aided Detection Markings: Two Schools of Thought. J Am Coll Radiol. 2015 Nov 1;12(11):1134–5.



Your point of replacing a second radiologist stood out for me. It highlights the need for a “human check” in healthcare that is reinforced with the “ALL” example. As an adoption technique, continuing the pairing model may assist in the confidence boost for physicians as well as improve the accuracy.