Ginger.io: striking a balance between humans and technology in mental health

Finding the right balance between human services and technological complements may be the key to creating and capturing the most value in mental health
Challenges in mental health
In the U.S., one in five adults experiences mental illness in a given year [1]. At nearly $200 billion in lost earnings per year [2], the associated economic impact is undeniably significant, but almost 60% of those experiencing mental illness today are left untreated [3]. The field of mental healthcare desperately needs to improve outcomes, and digitization has immense potential to transform it by connecting patients, providers, services and data in innovative ways.
Historically, patient-reported outcomes (PROs) on mental, physical and social health status were the primary inputs used to assess a patient’s risk for mental health issues and facilitate clinical decisions [4]. The incomplete and biased nature of PROs often led to costly repercussions when diagnoses were missed or delayed. However, obtaining continuous data on patient health-related behavior was difficult and costly, involving proprietary hardware or labor-intensive monitoring [4].
Harnessing big data and machine learning to disrupt mental health delivery
Ginger.io’s business model is built on obtaining and analyzing data that is timely, objective, and much less costly to collect. The company monitors patient behavior through smartphones and provides timely, objective data to providers. Providers are empowered to intervene effectively, boosting preventative measures and lowering overall costs (e.g., before patients fill up ERs or run up medical bills). Therefore, the business model targeted hospitals and provider groups as customers, since they bore the “financial risk” of poor outcomes [5].
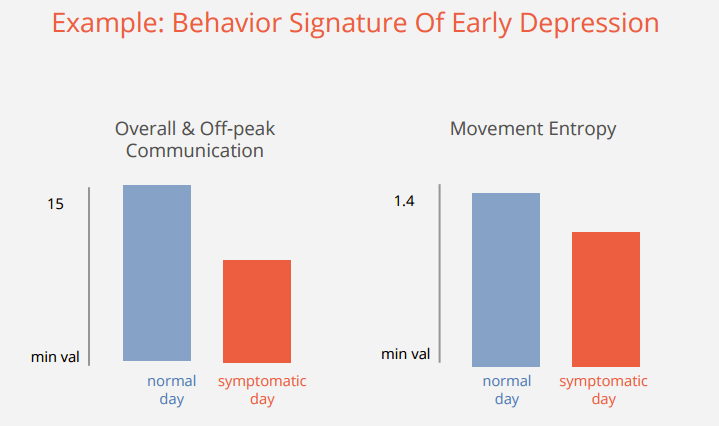
By amassing and analyzing large sets of “passive” mobile data, Ginger.io can detect if a patient with mental illness is acting symptomatic [6]. The company uses machine learning to detect complex patterns of behavior across multiple dimensions and predict when a user may need help. For example, a sudden decrease in social interactions (e.g., reduced volume of calls or texts) or physical activity (e.g., less movement captured by motion sensors) could signify that a user with depression is experiencing problems. When the app detects unusual patterns, it promptly notifies both patient and provider to take action as needed [6].
Other key components of the operating model included:
- Establish credibility through scientific validation – In order to attract and sell the platform to top-tier providers; Ginger.io must deliver significantly improved outcomes [7]. To that end, the company launched several trials and pilots with over 25 leading institutions and academic centers across the nation. [6].
- Build analytics pipeline to ensure data platform improvement – Ginger.io has already gathered and processed over 600 million hours of data from over half a million people with anxiety and depression [8]. As behavioral patterns are very individualistic, Ginger.io’s algorithms allow some degree of customization to create better predictive models. With this capability built into machine learning algorithms, the company can make continuous improvements and learn from mistakes [8].
- Target higher-acuity, care-intensive conditions to demonstrate value – For example, Ginger.io enabled UC Davis to improve early intervention for youth with psychosis which has historically involved expensive patient assessment and monitoring [6]. The company also partnered with McLean Hospital to reduce readmissions of hospital patients with schizophrenia [9].
Shifting gears
In spring of 2016, Ginger.io announced a change to their business model [8]. Instead of targeting providers and just offering the data platform as a tool to enable interventions, the company decided to go after employers and payers instead. Under this new model, employers and payers would purchase Ginger.io services as a corporate benefit for employees and members.
Ginger.io’s mission remained mostly unchanged: lower overall costs to employers and payers by improving members’ well-being through preventative and responsive measures. However, instead of operating as a “connector” between outside providers and patients, Ginger.io transformed into a licensed medical provider to directly deliver holistic mental healthcare to patients [10].
Consequently, this new business model meant substantial changes to the operating model:
- Build digital exercises and tools – Digitized exercises (based on cognitive behavioral therapy, mindfulness, etc.) provide patients with self-management tools [8]. Ginger.io also built robust communication tools (e.g., video conferencing, secure messaging) to facilitate relationship-building between Ginger coaches and patients.
- Shift to a “high tech, high touch” approach – Ginger.io incorporated personal coaches into the core product offering, complementing existing data platform and in-app exercises [11]. Coaches directly interact with patients, manage patient progress holistically, review patient data, and serve as an referrer for more specialized care (e.g., licensed therapists, psychiatrists) [11].
- Target lighter-acuity patients instead of clinical grade cases – Focus on anxiety and depression which are more prevalent and better suited for the new product.

How to include human care in a scalable manner?
Ginger.io’s business change raises some interesting questions. Why has the company evolved from a data platform to a licensed medical provider? Being a care provider requires more human capital (e.g., hiring coaches and licensed medical professions) which may not turn out to be a sustainable business model. It’s still too early to say if companies see value in Ginger.io’s service and how willing they are to pay for it.
Though this shift may seem less scalable and more difficult operationally, it may also be a reflection of limitations in technology. Perhaps technology alone is not enough to completely replace the human component in mental health care – at least not yet. While self-help interventions are poised for digitization and mass distribution, human connection remains a critical element in mental health treatment. Therefore, the real challenge (and arguably, the biggest opportunity) is finding the right balance between human services and technological complements to create and capture the most value.
Word count: 821
Sources:
[1] Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health, September 2015, http://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf).
[2] Insel, T.R (2008) Assessing the Economic costs of Serious Mental Illness. American Journal of Psychiatry. 165(6), 663-665.
[3] APA “By the Numbers,” 7-27-2015.
[4] Callaghan, “Disrupting Health Care with Ginger.io,” True Ventures Blog, November 28, 2012, https://trueventures.com/disrupting-health-care-with-ginger-io/
[5] “mHealth: Ginger.io & Personal Zen – New Approaches To Data,” MobileCloudEra, July 1, 2014, http://www.mobilecloudera.com/mhealth-ginger-io-personal-zen-new-approaches-to-data/
[6] Matheson, “Mental-health monitoring goes mobile,” MIT News Office, July 16, 2014, http://news.mit.edu/2014/mental-health-monitoring-goes-mobile-0716
[7] Huang, “Ginger.io Raises $1.7M for Mobile Health IT, Rides Wave of MIT Media Lab Startups Trying to Understand People,” Xconomy.com, October 18th, 2011, http://www.xconomy.com/boston/2011/10/18/ginger-io-raises-1-7m-for-mobile-health-it-rides-wave-of-mit-media-lab-startups-trying-to-understand-people/?single_page=true#
[8] Madan, “Your smartphone, your therapist?” World Economic Forum, January 21, 2016, https://www.weforum.org/agenda/2016/01/your-smartphone-your-therapist/
[9] Comstock, “Ginger.io is working with UCSF, Duke, Partners on diverse pilots,” MobiHealthNews, November 06, 2014, http://www.mobihealthnews.com/37976/ginger-io-is-working-with-ucsf-duke-partners-on-diverse-pilots
[10] Ginger.io Employer Information Page https://ginger.io/employers/details/
[11] Rao, “Tea leaves and ginger: What does success mean for a digital health startup?” Health Standards, June 16, 2016, http://healthstandards.com/blog/2016/06/16/digital-health-success/



Great article. It sounds like this tool solves a genuine need for patients and providers, so I’m a bit surprised it didn’t get taken-up by providers (I’m assuming that’s the only reason they would pivot). Even in a FFS world, this seems like it would both create new revenue opportunities for providers (in the form of additional appointments) and improve patient outcomes. I’m not terribly optimistic about this working out in a direct-to-employer model. Employer premiums are already going up, so the cost is a problem. Mental health is also something that a lot of employers aren’t quite comfortable talking to employees about yet. Finally, there’s the creep-factor of your employer being even remotely connected to an app that closely monitors your personal behavior.
Great post – thanks for sharing! The big problem that I see with mental health services is the stigma associated with seeing a therapist. If we think about Ginger.io and other similar apps, their success in large part depends on helping people realize and admit that they need help. From the description of the app and its features, it does not seem like Ginger.io is focusing on solving this problem. I’d be curious to hear your thoughts on how technology can help people overcome this initial barrier.
Another problem that I see in this area is connecting people with the right therapist. Even though Ginger.io is now hiring coaches, I agree with you that it doesn’t seem to be a scalable way to solve this problem. I wonder if they can instead leverage the large network of therapists and mental health centers across the country to solve the discovery and matching problem.
It’s very interesting to hear about the company’s shift from high-acuity to lighter-acuity conditions/patients as what seems to be a compromise to ultimately achieve a sustainable business model. Beyond just demonstrating value, I wonder if the company’s initial decision to target high-acuity conditions was driven by the desire to address conditions that are more apparently severe (not to say lower-acuity conditions are not severe, but just less apparently so). Regardless, I still believe there is tremendous value in their first initiative in targeting high-acuity conditions and would hope that they revisit it in the future after finding sustainability in their new business model. One idea would be partnering with public agencies, the government, or hospitals to leverage the reach that the company will (hopefully) have.
Really interesting post! Despite the risks of changing their business model to a higher-touch model, I think the contact with actual coaches is very important to establish trust with mental health patients, especially because mental health conditions can be very isolating to the patient. I would be curious to see some data on how member volume has changed since they introduced more high-touch elements.
One major concern I have for this type of digital mental health platform is the degree to which Ginger.io is held responsible/accountable for their online patients’ health. For example, what would happen if Ginger.io detects that a patient is sliding into a major episode of depression with risk of suicide, and they are prompting the patient to see a professional, however the patient refuses to do so. How would Ginger.io approach this issue? Who is liable?
One potential solution to the scalability challenge could be to build a network of external providers that are trained to use Ginger.io. In a way, this would be similar to how Uber selects and trains drivers to partner with. But in the case of Ginger.io, the screening, training and performance monitoring would have to be much more strict. This would reduce the needed capital and could help Ginger.io to grow faster while maintaining control over the quality of the service.
Terrific post Steph! I find Ginger.io’s current business model much more compelling, especially in their decision to position themselves as a mental health partner for employers and payers. I worked in financial services, where a series of high-profile employee deaths precipitated greater focus on and investment in employee wellness. However, given the stigma associated with mental health, most, if not all of the attention was given to physical wellness, with emotional and psychological needs relegated to an afterthought. I think the ease of Ginger.io’s communication platform is particularly valuable to a large number of patients who previously felt uncomfortable about seeking in-person treatment or were simply unable to receive treatment due to work schedule constraints. Coming from an industry where employees are already being offered financial incentives to monitor their physical well-being, I am hopeful that Ginger.io can shed light on the importance of mental wellness.
This is a thought-provoking analysis. Ginger.io is taking an interesting approach in tracking “passive” data via a mobile phone. I wonder if they could also leverage external sensors to further help evaluate patient health status? While doing research for my post I came across the CareCensus platform (http://www.usa.philips.com/healthcare/resources/landing/caresensus) which integrates a high touch interaction model with in-home sensors that can detect when a patient is experiencing distress. My main criticism of the Ginger.io model is that it is overly reliant on mobile phone use as a proxy for good health. As the population ages, more and more patients will experience mild cognitive decline and mental health issues. These patients may not use their phone on a regular basis, decreasing the value of a phone as an input source. I think there is an opportunity for a wearable device that can be integrated into the Ginger.io platform, and which extends its utility. There is research to suggest wearable technology could be used to greater effect in this context (Hentschel, M. A., Haaksma, M. L. & van de Belt, T. H. Wearable technology for the elderly: Underutilized solutions. Eur. Geriatr. Med. 7, 9–11 (2016).)