Dare to dream: A world without lancets

All around digitisation of blood glucose monitoring
Living with diabetes requires enormous lifestyle changes. Once diagnosed, changes in food, exercise and medication habits are necessary to avoid complications. Keeping blood glucose under control can be challenging, with many factors such as stress, exercise, or a simple illness driving glucose levels out of control.
The most dangerous effect of short-term loss of blood sugar control is hypoglycemia, or simply hypos, which can lead to a loss of consciousness as a result of extremely low blood sugars. Symptoms often include confusion, feeling weak and a tingling sensation in the fingertips. On the other hand, continuous high blood glucose can have serious long-term consequences.
Blood glucose monitoring: The traditional way

The traditional way of measuring blood glucose involves a lancet (small needle) that pricks the fingertip, after which a small drop of blood is loaded onto a small machine, generating a reading (See figure 1). Doctors recommend testing blood sugars several times a day (ranging from 3-10 times), usually at least before every meal. However, despite being a relatively simple procedure, many patients do not check their blood sugars. Underlying reasons for this behaviour are psychologically complicated, but include a lack of motivation, perception issues, and inconvenience around needles and pain1. A study by Diabetes Self Management found that 21% of adults with Type 1 and 41% of insulin-dependent Type 2 diabetes never checked their blood sugar levels2.
This lack of control has lead to poor self-management of the condition, leading to complications that are not only detrimental to the patient, but also a huge cost burden on healthcare providers. The American Diabetes Association in 2013 estimated that the cost of diabetes in the US has risen to $245 billion, a 41% increase over a five-year period.3
Continuous glucose monitoring (CGM)
Players in the diabetes market have long identified the need for continuous glucose monitoring (CGM). In other words, a device that would continually monitor blood sugar levels and alert the patient when needed, and that would not require all the steps and appliances described in Figure 1.
One such example is Dexcom, which comprises of a small sensor that is placed just under the skin to monitor blood glucose levels, the direction it is moving in and how fast (See figure 2). Glucose data is then sent wirelessly every five minutes to the patient’s iPhone or any other receiver via Bluetooth®4. Glucose levels are then shown in vivid colors on the Dexcom App and the data is easily compiled and shared with healthcare professionals.

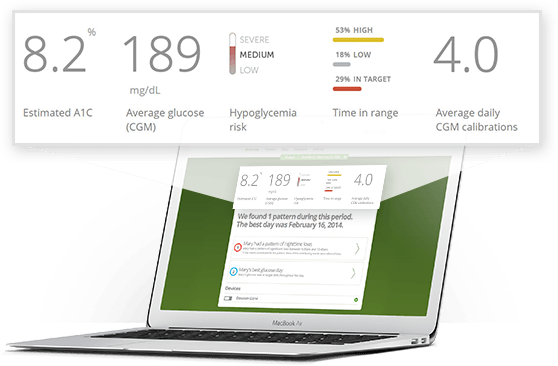
Apart from the Dexcom G5 mobile app that provides real-time glucose data and trends, Dexcom also offers CLARITY5, a diabetes management software that helps assess the user’s health by aggregating information on blood sugar highs, lows, daytime, nighttime and best day. The software also provides an estimate of A1C levels, which is a three-month average of blood glucose concentration (Figure 3).4 While Dexcom is widely used in the US, an equivalent device is offered by Abbott laboratories in Europe called the Freestyle Libre.6
Not only have the CGM devices such as Dexcom been instrumental in maintaining patient control over blood glucose levels, but they have also had profound impacts on two particular user groups: hypo unaware patients who have lost all sensations associated with hypos and simply cannot feel it anymore,7 and parents of children living with diabetes, for whom Dexcom has provided a great peace of mind, allowing them to monitor their children’s blood glucose remotely.
Drawbacks of current CGM devices
The primary drawback of both Dexcom and Freestyle Libre is invasiveness: both devices require that a sensor be placed under the skin, with the device being continuously attached to the user. This not only creates a risk of infection at the site of the sensor, but also harbors limitations on playing sports and clothing. Both devices have also caused allergic reactions in a significant number of users (personal communication, diabetes forums), are expensive, and need replacement every 1-2 weeks. Therefore, while CGM is always better than finger pricks, there is scope to look forward to yet more advanced monitoring systems that are less invasive.
Dare to dream: a world with non-invasive CGM?
Word Count: 679
References:
[1] Ong, W., Chua, S., Ng, C. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study (2014) Patient Prefer Adherence 8: 237–246
Web: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931581/
[2] Diabetes self management: http://www.diabetesselfmanagement.com/managing-diabetes/blood-glucose-management/ten-good-reasons-to-hate-blood-glucose-monitoring/
[3]American Diabetes Association: http://www.diabetes.org/advocacy/news-events/cost-of-diabetes.html
[4] Dexcom CGM: http://www.dexcom.com/continuous-glucose-monitoring
[5] Dexcom CLARITY: http://www.dexcom.com/clarity
[6] Freestyle: https://www.myfreestyle.com/freestyle-freedom-lite-meter
[7] Hypo unawareness: http://www.diabetes.co.uk/hypo-unawareness.html



Farhaneh,
Thanks for sharing information about a problem that many people in the world could relate to. I like Dexcom’s new technology since it uses charts and allows information to be easily tracked over a period of time to identify trends. Another advantage of the new technology is the fact that patients don’t have to obsessively check their blood sugar 10 times a day; this obsession could easily cause more stress and anxiety which in turn would lead to diabetes becoming worse. Nevertheless, the fact that Dexcom is invasive (one could even argue that it is more invasive than the lancet) is a significant drawback in my book.
Recently, a company called Echo Therapeutics developed a new technology called Symphony CGM that is actually non-invasive (i.e. does not involve the use of a needle). I think this new technology is going to pose a significant threat to Dexcom and I am very curious to see how the latter responds to it. I think competition is a good thing and would lead to more and more innovations, which can hopefully benefit patients.
Source: http://echotx.com/positive-clinical-trial-results-of-echo-therapeutics-symphony-cgm-system-to-be-presented-at-the-74th-scientific-sessions-of-the-american-diabetes-association/
Thanks for this post! One of the key takeaways I got from your article is the importance of balancing several factors when evaluating glucose monitoring devices. With Dexcom, the firm seems to do a great job of addressing the issue of pain and inconvenience around traditional measurement devices, but unfortunately sees another side-effect of being more invasive to the patient. As this industry continues to research new methods of measurement/monitoring, it will be important for companies to understand what factors consumers prioritize most.
For example, there currently seems to also be several non-invasive, wireless devices that have just entered the market, including a device called GlucoWise. This device’s competitive advantage is its non-invasiveness, where the product is “positioned to gently squeeze the skin between the thumb and forefinger, or the earlobe to measure blood glucose levels” (http://www.gluco-wise.com/). However, a challenge that this company faces is the degree of accuracy that this device provides, given its surface-only measurement method. Both GlucoWise and Dexcom provide an interesting view into the trade-offs between different factors of using a glucose monitoring device. What will be interesting to see is whether a company can address all three of these factors simultaneously (pain/inconvenience, invasiveness, accuracy) when designing the next breakthrough device.
Thanks for the article! Knowing a few people who suffer from Diabetes (in particular, one friend who even in high school had to constantly be pricking himself/checking blood sugar), I see the real convenience in not having to so consistently draw blood. As I was reading the piece, I was wondering about the invasive nature of the device – something you addressed as the product’s key drawback. This leaves me wondering…how close are the efforts to actually do this non-invasively? Is there a great deal of research money behind this? If successful, it would certainly improve the lives of many!
This is a very interesting article. I would wonder if anyone in this sector has looked at nanorobotic solutions to this issue – that is, implanting a glucose monitor in the blood stream via a small instrument. While this of course elicits a whole new level of ethical concerns and concerns about invasive therapy, it would potentially minimize the risks of infection and the inconvenience on the patient. The below linked article gives some details about how this has been explored to targeted drug delivery in the human body, but has yet to really be implemented. Perhaps there is a happy medium that would enable this kind of robot – which does not need to deliver a drug which needs to be FDA approved – to leapfrog the robots that are currently being considered for use in human bloodstreams.
http://www.theatlantic.com/technology/archive/2015/08/nanobot-treatment-doctors-cancer/400613/
Frahaneh thanks for sharing and informing us about the conditions and treatments people living with diabetes go through.
I found particularly interesting the application this type of Continuous Glucose Monitoring systems can be used in children. After researching in some blogs many parents are concerned that many children are not able to identify when their blood sugar is dropping, either because they don’t feel it or because they are too young to properly express it in words. And the parents that have been using CGM have expressed how now they have more context about the numbers of sugar in the blood of their children, helping them make better decisions about insulin dosing and treating lows. (1)
But I also learned about the problems you were mentioning plus other common ones like false alarms. A lot of patients have gone through periods of concerns given a sensor false-alarm, however with more use they have found that the sensor becomes inaccurate in certain conditions, like at the end of its useful life.
1. http://www.diabetesforecast.org/2013/jun/the-pros-of-cgms-for-kids-and-parents.html
This is such an important realm in which technological innovation can have profound impacts on patients, providers, and our healthcare system at large. The number of patients I’ve helped care for who suffer from poorly-controlled DM and the vast number of complications is causes has left me very discouraged. Getting patients to reliably track their blood glucose is such an uphill battle for the reasons you stated in the article, and yet the complications that arise later result in profound morbidity and mortality, costing patients huge sums and putting huge financial strain on private payers and medicare alike. Once we have a revolutionary breakthrough for management of DM, like the technologies you outlined, the gains in years of life, quality of life, economic productivity, and healthcare savings will be immense–especially given that diabetes affects roughly 10% of the US population.
From what I could gather in a very brief literature search, it seems like there is a bit more improvement needed in the technology–since the CGM machines monitor glucose levels in the interstitial fluid (vs blood using finger-stick blood glucose monitoring), the readings are only accurate ~75% of the time since there is a delay in equilibration of diffusion between fluid compartments. [1] I agree that the technology is perhaps most useful for those who are at risk of unkowingly becoming hypoglycemic, particularly children, but it seems that the readings have a lot of accuracy during times of exertion/exercise (which kids would be prone to). [2] I, too, am interested to see how the proliferation of non-invasive technologies (which Mary eluded to above) will impact the development of the CGM tech, and whether or not accuracy vs cost efficiency wins out.
(1) https://www.ncbi.nlm.nih.gov/pubmed?term=18715215
(2) https://www.ncbi.nlm.nih.gov/pubmed/27356172
Thanks Farhaneh, wonderful article. Didn’t know that we have made such advances in teh field of glucose moitoring. An issue which affects many in the world, I guess we are in the right direction and soon through more advancement in the field, would help eliminate some of the cons posed by these new technologies.
Very interesting thought, even with being invasive POC (point of care) testing and testing based on micro units of bloods itself has such vast and over-reaching implications. As far as I understand blood glucose is one of the few parameters that be tested using blood drawn from extremities, recent ordeals of Theranos seems to have conclusively shown that we are not close to a solution! I do feel that such technology, however, has the potential to disrupt both human health as well as the mammoth global diagnostics industry.